Hip Arthroplasty
1992/11/01 Agote, Jose Antonio Iturria: Elhuyar aldizkaria

Hip arthroplasty consists of replacing the surface of the hip joint with artificial materials. This joint, like any joint, is sometimes affected by different diseases on its surfaces, destroying the cartilage of the articular surface or the subcondrial bone. All this produces in the patient three basic functional effects that he suffers in his daily life: lameness, pain and loss of movement.
History
Complete hip arthroplasty is the most commonly used joint reconstruction method worldwide.
The evolution of hip prosthesis materialized in three areas: the improvement of prosthesis designs, the improvement of manufacturing techniques by using increasingly suitable materials and the deeper knowledge of hip mechanics by improving surgical techniques.
The manufacture of the first prostheses began in the last century, but due to the low quality of the raw materials (lead, aluminum, zinc, leather, boli, boxwood,...) were total defeats.
The first prostheses were used to modify one of the two surfaces of the joint and the surface was only the head of the femur (only changed the femur part of the hip without changing the cotilo). In this line the first prostheses of modern materials began. The femoral steel and chromoconalto prostheses date from the fifties. These prostheses changed the surface of the femoral head like a cap. Therefore they were called “cup prosthesis”. The Judet brothers began placing acrylic prostheses in the 1940s. In the sixties ceflonic teflon prosthesis began to be placed without any results.

By then the new metallic prostheses were presented, but instead of the cap or designer they had a metal root to plant inside the spinal cord canal. The first examples were Thomson and Moore's prostheses.
But all these femoral stents had the same problem: since one of the two surfaces of the joint was replaced, the play was performed between the cotilo with cartilage and the metallic prosthesis. In this way the cotilo quickly eroded and within a few years the mines recovered. Therefore, in view of this problem, the replacement of both surfaces was considered as the most appropriate solution. Thus began the generation of complete prostheses to date. The first generation of complete prostheses were Urist, Ring and Mckee-Star prostheses. In these prostheses the two joint surfaces were metallic; high friction prosthesis. The consequence was the relaxation of the prosthesis and the appearance of new ailments.
When the entire prosthesis began, another problem had to be solved: studying and selecting materials that supported joint movement and friction. And in this sense we must consider as pioneers the work of Sir John Charnley, who explored all fields of hip prosthesis.
One of the advances achieved by Charnley was to find the consistency of the union between the prosthesis and the bone. He obtained this point with cement or acrylic cement, polymerizing or hardening at natural room temperature. When analyzing the results of a new prosthesis model, Charnley's prosthesis is taken as a reference point.

The studies of recent years and the new current models go by two ways: the way of study that aims to obtain prostheses without acrylic cement or acrylic cement and the way of acrylic cement, trying to achieve improvements in cement.
Prosthesis components and materials
Since Charnley presented his prosthesis in 1959, it has undergone numerous transformations in its design, materials and solutions and kneading media in the bone. As it would be long and complicated to list all the changes and models that have appeared in the market, I will choose a general model and describe the most common ones that exist in it.

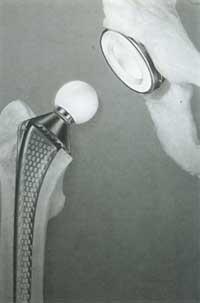
In any current prosthesis, the two components that suffer friction, the supporting components and the joining systems should be differentiated.
Two components subjected to friction
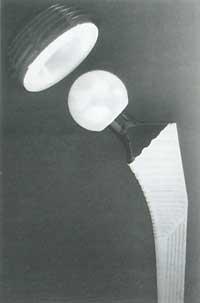
The semispherical cup or dome of the cotilo and the spherical femoral complements.
The main problem that has had to be solved in this field has been the achievement of a low level friction between the components, reducing as much as possible the wear that would generate the use. Four different binomials or pairs are used and are used in the following accessories: metal/metal, plastic/metal, plastic/ceramic and ceramic/ceramic. Of these four models, metal/metal is currently totally excluded.

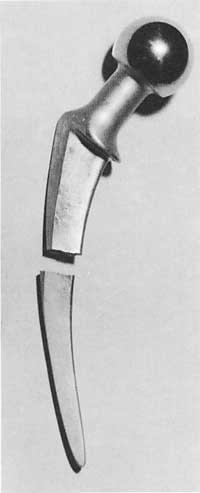
The head is placed in the root that is inserted into the femur channel. In some prostheses the head, neck and root form one piece, but in most cases it has two different pieces.
Components support
It is the transmitter of weight or forces. It is the root of the prosthesis and is almost always metallic. This component covers the distance from head to bone (transmitting loads) and is placed in the spinal cord canal. It is the aspect that has suffered the most changes.
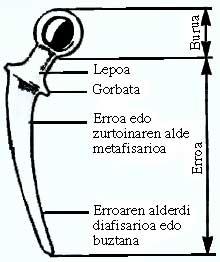
The root is divided into four parts: neck, tie (it does not appear in many models), metafisaria part of the root (underlying part) and diafisaria part or tail of the root.
The design models of these last two parts of the root have increased considerably in terms of length, curvature, cutting shape and surface nuances.
The root is always metallic and among the metals the most used are steels, chromium cobalts or stelites and titanium.
Joining systems
Prosthesis accessories described so far must be attached to the bones of the body (cotyl and femur) for the transmission of forces.
Depending on how the prosthesis is associated with the bone, there are two prosthesis systems or sets: those that use acrylic cement to perform the bonding and prostheses that have been imposed to pressure without cement.
Charnley pioneered the use of acrylic cement in his prosthesis. In fact this material is a polymethacrylate methyl resin to which some drawbacks are attributed: the heating that occurs in the hardening reaction at the time of its placement, the toxicity, fragility and the breakdown of cement that occurs over time due to its low resistance to fatigue. Some are real, others more theoretical.
In the beginning, acrylic cement was considered a means of gluing the prosthesis, so it was considered that the more cement was placed the better. As it has become known and deepened in the experience it has been discovered that there is no adhesiveness. Its function is to perform the interface between the prosthesis and the bone, that is, the adaptation. According to this theory, cement should be used prudently and as little as possible, dispersing it homogeneously at the interface between the prosthesis and the bone.
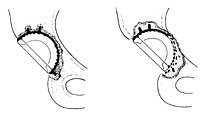
In the case of prostheses using biological fixation systems, the prosthesis metal is attached directly to the bone. About twenty years ago this system began. The surface of the prosthesis is filled with wrinkles and pores. Thus the bone, when it grows, can hold firmly to the prosthesis entering pores and wrinkles. Consequently, the joint between the prosthesis and the bone is achieved.
The introduction of the bone to the prosthesis surface requires a primary temporary attachment of the prosthesis, which is obtained by pressure, by attaching the prosthetic part to the bone by means of screws or by direct screwing of the prosthesis part. In these cases, the burden of the prosthetic carrier member should be avoided during the development of the biological or secondary liaison.
Indications of hip prosthesis


Initially, the indication to place prostheses on the hip was a disabled patient with pain older than 65 years, when previously no positive results were obtained with other measures of an ezkirurgic nature.
The role of change was of secondary importance. When good results began to be described, indications began to spread to other diseases. See table Hip diseases in which the entire prosthesis is indicated.
On the other hand, it is necessary to know that total arthroplasty (complete prosthesis) is not the only surgical treatment that can be performed in the hip who suffers the pain.
Before recommending any reconstructive hip intervention, non-surgical measures should be used to the final limit (weight loss, anti-inflammatory medication, circulation with a staff and other medical orthopedic measures). These measures often relieve pain, avoiding or delaying the need for arthroplasty.
Therefore, the placement of prostheses would be indicated, although the pains taken by normal analgesics prevent the patient from leading a normal life. Pain is the first and complete surgical indication. Therefore, patients who are losing hip movement have no indication of placing the prosthesis if they have no pain or pain.
Contraindications
Arthroplasty is a high-level surgery. Complications and mortality should be considered (1%-2%).
Therefore, before recommending arthroplasty it is necessary to investigate well the condition or general health of the patient, especially kidney, heart, liver and brain diseases.
Specific contraindications for arthroplasty would be:
- Active pre-hip infection.
- Another body infection (urine, lung, skin,...)
- Onset of diseases of rapid bone destruction (deep osteo-porosis, generalized progressive osteopenia,...)
- Neurotrophic joint. Progressive neurological disease.
- When they are affected by cancer and in the hip area there are important bone deficiencies.
Average prosthesis duration

One of the most characteristic problems of hip prosthesis is the prediction of the duration of the prosthesis.
All published studies show excellent results for the first three years. In the medium term the results are very good. In a five-year period its success ranges from 80% to 90%. The percentages of failure begin to increase from eight years. Functional degradation begins in cases of 20-30% from the intervention until the eighth year, due to the relaxation of some component of the prosthesis.
Measurements of long-term results have some drawbacks, since almost all patients are elderly and have very low physical activity. On other occasions, loss of the patient's fingerprint or death from another disease cannot determine how long it could last.
It is more significant to analyze the duration of the prosthesis implanted in young people, since in these cases life expectancy is greater and the physical activity required to the prosthesis during those years is much greater.
Statistics show that the risk of relaxation in young people is 20% higher than usual. These results justify the need to be cautious before putting a prosthesis on a young person.
Complications
It is necessary to say that thanks to the advances of medicine the number of complications has been considerably reduced.
Some complications of all arthroplasty have to do directly with the intervention or with the same technique. Others are complications related to the patient's overall health.
All the data we have about the complications of the technician or the arthroplasty itself come from studies carried out in cemented arthroplasty. As
for the complications of arthroplasties without cement, for the experience of a few years we still do not have concrete data and are limited to three points: rupture of the femur by putting the root to pressure, loosening of the cup or root of the cotyl and disappearance of the bone of osteolisis or metaphysics of the femur.
of the second type of the cotilo prosthesis: divided acrylic cement and displaced prosthesis. Osteolisis is important.
The complications that may occur are: ingestion rupture (which is shrinking), prosthesis dislocation (which rarely occurs), postoperative coacles (which has been greatly reduced), postoperative urinary infections (which are easily repaired and in the short term), postoperative prosthesis infection (which is the most feared complication, but which occurs in a 0.5%-1% heterogeneity), delayed infection (about 10%). It can prevent the movement of the prosthesis, to a different extent depending on the case. It is produced by 5%. ).
The future of prosthesis
The future of hip prosthesis is currently being worked in two areas: research and design of new materials and operational technical improvements.
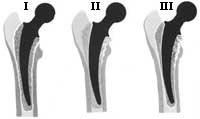
Lasaipena I: lasaipe between bone and acrylic cement.
II. lasaipena: lasaipe between acrylic cement and metal root.
III. lasaipena: sum of previous types of lasaipes
The area of new materials is researching in three areas: in the reduction of friction, in the components that serve as support and in the union area or fixing system.
The operational technical improvements are based on three criteria: achieve a good architectural reconstruction of the hip, achieve the least aggressiveness of soft tissue and reduce the risk of complications.
Particular attention should be paid to reducing the risk of operating technique. In France, for example, over 50,000 hip prostheses have been placed in recent years. The future of these prostheses will undoubtedly depend on the materials, but largely on the quality of the prosthesis implantation technique.
Surgical technique is not learned in books and advertising papers. It is the result of constant teamwork that requires good knowledge of anatomy, understanding prosthetic laws and rigorous critical vision.
About the prosthetic patient
Mentalities have changed in patients. 20-30 years ago the placement of the prosthesis was a menture by the number of complications that there were.
Today, we have entered the era of rutinization and much recognition and confidence in the prosthesis has spread.
A patient's desire to move in his car a month after the day of surgery has become almost everyday. Others want the prosthesis to start or continue to suit their tastes.
It is not possible to make an exhaustive list of all recommended and not recommended movements and tasks at the moment. When the patient is hospitalized, it must be “educated” indicating which attitudes to avoid and which potentiation to adopt so that postoperative locations do not occur according to the prosthesis model.
Sports that can cause shocks in everyday life should be avoided. The limits of exercise or sonorization are not determinable, since there are large differences depending on the cases.
Hip diseases with total prosthesis indicated
- Arthritis:
a) rheumatic
b) juvenile rheumatic arthritis (Still's disease)
c) ankylopoietic spondylitis
d) degenerative arthritis:
– primary
– secondary or consecutive:
– epiphysiolisis of the femoral
head – dysplasia or hip dislocation
by birth – traumatic
dislocation – coxa launa (Leeg —calve— Perthes disease)
– traumatic rupture of cotyl
– hemophilia - Abascal necrosis (from the head of the femur):
– as a consequence of fracture or localization
–
idiopathic – epiphysiolysis of the femoral head – hemoglobinopathies (sickle cell disease) – kidney disease – cortisone – alcoholism
– divers
disease – lupus
– Gaucher disease - Pseudoarthrosis: fractures of hip bone or femoral neck that affect the femoral head
- Pyogenic arthritis or osteomyelitis:
– hematogen
– postoperative - Tuberculosis
- Mud or by birth
- Hip fusion (ankylosis)
- Failure of previous operations: a) osteotomy; b) cup arthroplasty; c) partial or cephalic prosthesis; c) Girlestone technique; e) failure of the total prosthesis previously placed.
- Cancer that collects cotyl or femoral head
- Hereditary diseases (e.g. acondroplasia).

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia