Artificial heart: miracle or dark business?
1986/12/01 Arrojeria, Eustakio - Elhuyar Zientziaren Komunikazioa Iturria: Elhuyar aldizkaria

On this occasion we address a goal that has become the dream of the human being. As is known, human beings have always evolved towards overcoming the limits of ourselves and one of them has been the elimination of diseases or enemies of our own health, or the replacement of others more beneficial even if it were not. Research closely linked to the heart is part of this field.
But, in any case, getting it is really difficult. And is that the complexities of fabrics that have a life, that generate a great drawback in substitution, make it very difficult to get an effective and useful replacement. Therefore, talking about artificial hearts in an instant seems like a spell, even if we know and do not know that the heart is a simple pump of blood distribution, as previously thought, the location of the amine and feelings.
At a time when heart transplantation has spread around the world, although the success achieved is controversial, the fundamental role of unattainable heart muscle in replacing the artificial machine, despite the difficulties of the machine, has been expanding hope. Moreover, the results obtained are not of great performance, although in 1982, in the research of the artificial heart Jarvik-7, 350 million dollars (60,000 million pesetas) have been spent. These are the first steps that are being taken in this field and may at some point, investing more money and in time, be able to succeed.
But some begin to worry about this, because, as is known to everyone, in mute medicine a machine is needed, and many have more priority than those of the artificial heart. How can so much time, money and wisdom be invested in these investigations? Moreover, there are people who have already denounced that private researchers working in this field want to create a dark business. A lot of money is already being invested and as you can see, in the short term it is not profitable, but in the long run it is. That is, they would be the only providers in this matter.
Despite all this, this is still underway and, in addition, in the United States, leading companies in this area face the sponsorship of private initiatives. For its part, Saudi Arabia has promoted the experimental module developed by the French doctor Lapeyre in collaboration with the airline Aérospatial. American doctors Kolff and Iarvik of the University of Utah and Japanese doctors Zorrsu are funding their Jarvik-7 project. Currently, and with a doubtful success, they have been placed in three patients. The annual budget of these researchers already exceeds 50,000 million pesetas.
Initially, as a result of Dr. Barnard's first heart transplants, surgeons began to dream of an artificial heart that would completely limit or exclude crushing problems. However, a disproportionate technological challenge arose: the machine had to respond to extremely demanding conditions from the point of view of hair, weight, duration, energy, anatomy and operation.
Kolft and Akutsu first compressed air model was tested with animals on 12 December 1957 and the one that survived the most spent 90 minutes. In 1959, for its part, a veal named Fumi Joe lasted 221 days, which used a prototype laboratory that served as a guide to the current artificial heart Jarvik-7. Ten years later, in May 1969, the era of artificial hearts applied to men began.

Denton Cooley, a doctor at the University of Houston, Texas, established a mechanical heart of compressed air in a forty-seven year old person. This heart was regulated by the Argentine Domingo Liotta. The patient spent 54 hours with this artificial heart while transplanting the natural heart. Today and a half later he died from pneumonia. In this case, the artificial heart served to maintain the necessary time until obtaining the natural heart for its transplant.
This aggravated the debate: if you save a few hours, why so many interventions? Do we not have men as rockets? But Dr. Cooley defends himself by saying that his patient had an unavoidable opportunity, that he would never have had.
At this time, revegetation surgery faced the unfortunate consequences of the crushing of the body. And the truth is that with so little clinical experience in this type of operations there were no significant reasons to carry out this decision. The scandal affected Cooley because he did not get official permission to operate. As a result, the official grant and teaching lost the permit and, at the same time, his job in the hospital, that is, was expelled.
But private enterprise took the place of state power and twelve years later, in 1981, Denton Cooley continued his work. His sick, a twenty-six year-old man, remained three days with an artificial heart, even until the natural heart was transplanted. He died one week after the transplant. This initiative has suffered new convictions among doctors. However, trials in this field do not end with this; in May 1982, the University of Utah team introduced the mechanical heart into Barney Clark's chest.
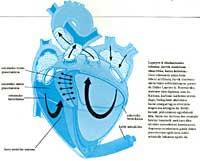
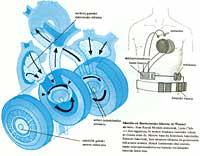
This, with a disease called dessert cardiomyopathy, usually lasts very little (a few days). The transplanted artificial heart was a durable model called Jarvik-7, as there was no human heart at hand to be transplanted and not expected. Surgeon William DeVries, part of the group of pioneer Kolff, operated successfully. But unforeseen difficulties arose due to the age of the patient and the poor condition of the cardiac and arterial vessels.
The artificial heart also presents some errors that must be overcome immediately and with all kinds of means. After the operation, the patient suffers a cerebral congestion as a result of the increased tension. Therefore, the patient remains sunk, does not feel like living and recognizes his desire to die before the doctors. In any case, Barney Clark survived 112 days (almost four months), but it must also be recognized that he was in a very bad situation.
The controversy returned to explosiveness levels and, after harsh criticism, the University of Utah decided to end the trials. But surgeon DeVries, as stubborn as Denton Cooley, convinced he was good of the system, moved to the Human Hospital of Louisville, located in the state of Kentucky. This hospital is the private center of a chain of hospitals that extends all over the world and that, as is known in the field of medicine, is designed to earn money. But as far as the patient is concerned, he is offered unique care and help, and on the other hand, the basic level of research and teaching that this chain has is very high. In addition, the economic and administrative procedures are detailed.
Therefore, taking into account these three sections, it could be an example of most public health systems.
Surgeon DeVries, at the Humana Heart Institute in Louisville, performs a permanent artificial heart transplant. This was the second operation carried out by him (the fourth one carried out in humans). On 25 November 1983, Willian Schroeder, with more than forty years of cardiomyopathy, was given a mechanical heart called Jarvik-7. It was faster and more effective than Barney Clark's operation. The latter managed to exceed a year and a half, but with great drawbacks.

On February 17, 1984, DeVries transplanted the third permanent artificial heart into his personal competence. Murray put him to Haydon. He is a man of fifty years. But, as is known, Haydon found himself in a critical situation, having survived for quite some time on the artificial airway. However, it also managed to exceed a year and a half.
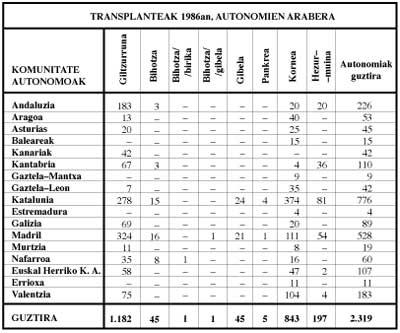
As you can imagine, the contradictions and the shots have not ended for the moment. Those who defend transplants in the human heart, since it began to use cyclosporine, good (for about six years approximately good), claim to dominate largely the negative effect of trampling, that is, say that the body does not have an artificial heart as before, that is, that the body does not reject the artificial heart as before. In the United States, more than 200 transplants are performed each year, of which 80% have a year-long hope and 50% have a 5-year hope.
If we take into account that twenty years ago he had a technique that had no solution, we must recognize that much progress has been made. Therefore, and using the words of the supporters: What are the reasons for starting the research of a new technique, less effective and more expensive, at a time when the technique we have almost mastered? Jarvik, inventor of the mechanical heart that bears his name, wrote in 1983 that it was necessary to wait another five or ten years to get a totally reliable cardiac prosthesis that could live like any other human being.
Decries, for his part, goes further in his statements. In this sense, the doctor must, in principle, analyze and accept the use of all the resources in his hands in critical moments, without rejecting any of them, even more so when it serves the progress of medicine and, incidentally, human lives can be saved in the future.
But the problem that is discussed in depth, in addition to fertility and capacity, is the problem of selection. The advancement of technology in the new era offers unavoidable opportunities, so the doctor and medicine in general are forced to make some selections. The problem has become uncomfortable. The curious military solve this problem with the method of classification during the war.
For example, minor wounds are neglected, only healed, even those that are very bad (there is no time or means to save them), and only intermediates will be treated. However, civil medicine cannot act in any way. But this is not an anti-choice medicine and the problem is still there. Who should be elected?
Should they be patients with positive prediction that offer a more reliable recovery? Or should patients with less hope be helped on a priority basis and in principle, although the possibility of success is very limited?
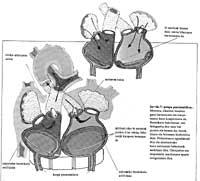
However, for the moment it is evident that the artificial heart, technologically, is not fully prepared. The conditions for obtaining an ideal cardiac prosthesis are at the moment far away, because, curiously, physiologists have not yet come to create a model that fully responds to the dynamics of the functioning of the heart. Moreover, the human heart has not given us all the details of his wonderful work. Therefore, the construction of a mechanical heart that wants to be equivalent and its proper functioning is a difficult task.
On the other hand, no suitable materials have yet been found. The material must be both solid and biologically integrable to form the possibility of coavid formation. These were some of the causes of the brain attacks suffered by Schroeder and Haydon. Materials obtained through the union of different plastics and alloys are currently used. Over time, the polyurethane of the diaphragm is calcified, so in the short term trunk fibers and textiles are generated around the apparatus.
The valves of the Jarvik-7 of the ridge, having to withstand a greater effort than that imposed by the human heart, weaken and cause problems. Current researchers lean towards carbon-carbon material. It is a material composed of special technology. In addition to being resistant to erosion, the human body does not frustrate it, since porous carbon merges with living cells, thus producing new tissues around the prosthesis.
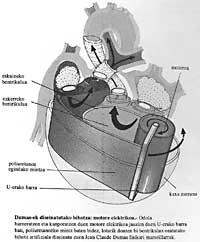
When the final implementation is proposed, the material conditions become very strict: unexchangeable valves, engine performance around 90%, consumption less than 5 watts, resistance to membrane wear, total reliability of electronic systems… The weight of the motor is a very important parameter and is closely linked to the measurement. The ideal would be to achieve a complete implantation, combining the pump with the motor, avoiding any external accessory. The Japanese seem to be working on it.


But at the moment we are far from getting it. However, from the compressor that was applied to Barney Clark to its application to Schroeder there is a difference of 25 kilos within two years. However, this compressor weighed 161 kilos. As you can imagine, Schoeder and Haydon lived together with the compressor, but it was invented by the Germanic engineer Peter Heimes thanks to a six-kilogram capacitor that could get a break of two or three hours during the day. Apparently, nuclear power has been rejected (heat, waste, battery weight). They have also rejected the power obtained with the conventional electric battery, since they are unfaithful and short-lived.
The artificial heart Jarvik-7 does not take into account the thoracic area of the human being. Dekries selected patients who fit the heart and not the other way around. Clark, Schroeder and Haydon had a common feature: an abnormal chest, that is, a very wide chest. Artificial heart placement was no easy task.
All possible objections to the artificial heart will probably not impede its development. It is a medicine of prestige and not for all, more discriminatory than discriminatory. But, despite everything, it seems to have a future.
The war between defenders and detractors of the artificial heart seems to win the first. This heart machine seduces people. For private finance, the business that can be generated around good is tempting. This problem revives specialized industries and challenges space-related or aeronautical industries.
The symbiosis between engineers and surgeons and the mechanics of physiology and precision seems for the moment too fascinating a dream.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia