Pancreatic transplants
1994/06/01 Furundarena Salsamendi, Jose Ramon Iturria: Elhuyar aldizkaria
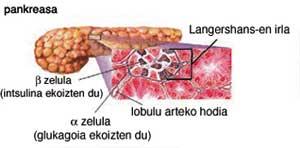
The insulin we need to metabolize glucose or sugar is secreted by a viscera called pankreas in the depth of the belly. When it is not able to produce enough insulin, the disease called diabetes appears, it increases the blood glucose level and causes damage to certain viscera and body positions (kidneys, heart, eyes, etc. ).
Some medications may be used to treat diabetes, one of which is also sold as a daily insulin puncture, but this time we will talk about pancreatic transplantation using data obtained from the journal "Lancet". Since Kelly demonstrated that transplantation could be effective in 1967, the use of this technique has spread to many hospitals. Over 4,000 transplants have been performed in the last 15 years, 70% since 1987.

Pancreatic transplantation allows the patient to be released from the daily injection of insulin, but to avoid the failure of the transplant an immunosuppressive treatment is necessary and the three drugs usually used for this produce unwanted effects: aciathioprine affects the bone marrow, cyclosporine can affect the kidneys and steroids can produce gastrointestinal bleeding.
It is understandable that a diabetic dreams of being free to take a medicine daily, but if he has controlled his diabetes with that drug, we cannot enter the aforementioned risk. On the other hand, if the correct administration of insulin does not allow the control of diabetes, an alternative should be offered to this patient. So when should the diabetic possibility of transplantation be offered?
In patients with ocular retinopathy it is observed that their situation is similar to that of patients who have spent 3 years and who have gone wrong in cases where the transplant has been performed. In cases of developed retinopathy, treatment is laser photocoagulation and transplantation is not the solution.
In cases where retinopathy has not yet developed, we should investigate whether insulin or transplantation is better. The effects of diabetes on nerves can improve with transplantation. Muscle forces, different sensitivities and autonomic functions can be partially recovered when the transplant is successful.
After pancreatic transplantation, renal function worsens during the first year and stabilizes. This damage is considered to be a consequence of cyclosporine toxicity. If they are analyzed by renal biopsy at 5 years after transplantation and compared with biopsies done to other patients treated with insulin for 5 years, there is no benefit. Therefore, pancreatic transplantation cannot be defended in order to improve renal function.
However, once the 10-year period has elapsed, it will be advisable to review it to check for long-term differences. The possibilities of transplantation to improve the effects of diabetes on blood circulation have not been properly studied and until the data is published nothing can be advanced.
Using data from an International Registry, of the 2,103 transplants performed in the United States until 1992, 71%, 66% and 59% still worked at 1, 2 and 3 years, respectively.
Taking all of these data into account, pancreatic transplantation cannot currently be defended. The only exception may be a patient who cannot be controlled with insulin and therefore is in danger of his life. Everything can change if the transplant result is improved, safer immune treatments are found, and transplantation is shown to be more effective in the adverse effects of diabetes.
The situation is very different when diabetes causes deep kidney failure, that is, when dialysis is needed to survive. In this case, a unified kidney and pancreas transplant may be performed. In addition, for unknown reasons, the survival of the pancreas is better than when only that viscera has been transplanted (75% survival a year). However, as far as double transplantation is concerned, many questions remain to be answered and good research must be done comparing double transplantation with simple renal transplantation.
The points to be taken into account in this study would be the quality of life of the patient, the greater hospitalization of double transplants and the greater number of incomes during the first year, the high mortality in those over 45 years, the higher economic cost. We must not forget that today, compared to double transplantation, if the donor is a living relative, the survival of the kidney is greater. However, the most important point to measure would be patient survival.
Finally, we cannot forget the transplant of pancreatic islets. The pieces of pancreas that produce insulin are called pancreatic islets and instead of transplanting the entire viscera, there have been transplantation sessions of those pieces. The biggest problem of this technique is that they are rejected and many research seeks to somehow overcome this problem. The best results can be obtained in the future by this route, as it avoids many of the risks involved in transplanting the entire pancreas.

Gai honi buruzko eduki gehiago
Elhuyarrek garatutako teknologia